
How can Lipodystrophy be diagnosed?
Generalised and partial lipodystrophy (GL and PL) are severe diseases with external signs that are visible and signs that can only be identified on examination.
Signs and symptoms may manifest differently in each patient and not all occur in every patient. Even the same form of lipodystrophy can show different physical and metabolic symptoms, both in type and severity. Therefore, the appearance of patients with generalised and partial lipodystrophy subtypes can vary greatly.
How is it diagnosed?
Generalised and partial lipodystrophy are rare diseases, most doctors have little or no experience with them. For this reason it may require consultation with different specialists, that can lead to a diagnosis. Here, the examination of the blood, the internal organs and also genetic testing play an important part. Some of the specialists that can help diagnose lipodystrophy are listed below.
Geneticists
Geneticists deal with the diagnosis of genetically determined, i.e. hereditary diseases. Many forms of lipodystrophy can be confirmed genetically. Genetic testing of family members with specific mutations can reveal potential lipodystrophy cases.
Lipidologists
Lipidologists are specialists in fat metabolism disorders. They have in-depth knowledge of hypertriglyceridaemia in particular. Patients with lipodystrophy exhibit high triglyceride levels.
Hepatologists
Hepatologists deal with liver disorders. Fatty liver is a common abnormality in lipodystrophy, that can lead to liver failure if remains untreated.
Endocrinologists/Diabetologists
Lipodystrophy patients often exhibit insulin resistant diabetes. Endocrinologists deal with the body’s hormone system. They are specialists in metabolic disorders such as diabetes. There are also endocrinologists who specialise in the treatment of metabolic disorders in children.
Nephrologists
Nephrologists deal with kidney disorders. Patients with lipodystrophy may develop proteinuria or impaired kidney function.
Gynecologists
Puberty problems, menstrual abnormalities, polycystic ovaries, hirsutism and fertility problems can develop in females with lipodystrophy.
Cardiologists
Cardiologists deal with the cardiovascular system and its diseases. Lipodystrophy can be associated with heart problems such as cardiomyopathy. Cardiologists are involved in the assessment and management of many cardiovascular complications.
Paediatricians
Geneticists deal with the diagnosis of genetically determined, i.e. hereditary diseases. Many forms of lipodystrophy can be confirmed genetically. Genetic testing of family members with specific mutations can reveal potential lipodystrophy cases.
If you suspect that you might suffer from generalised or partial lipodystrophy, then you should speak to your family doctor or paediatrician. Do not be afraid to request clarification of uncertain or unusual signs of illness, for yourself or your child. The following questions might help you:
Lack of subcutaneous fat?
Unusual fat distribution?
Insatiable hunger?
Diabetes mellitus that is difficult to treat? Insulin resistance?
High triglycerides in the blood? Fatty liver?
Acanthosis nigricans? Menstrual abnormalities? Protein in the urine?
How is it classified?
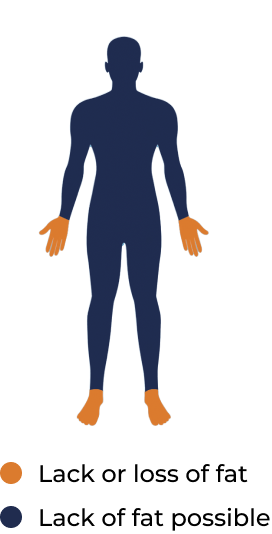
Lipodystrophy is always linked to a lack or loss of subcutaneous fat. There are also further visible and invisible signs of the disease like metabolic changes which can point towards lipodystrophy. The disease is classified into 4 main groups. First, there is the division between the fat being absent in the whole body (generalised) and only in certain parts of the body (partial). Both GL and PL are then further subdivided into congenital (familial) and acquired. Lipodystrophy is a rare disorder.
Generalised lipodystrophy (GL)
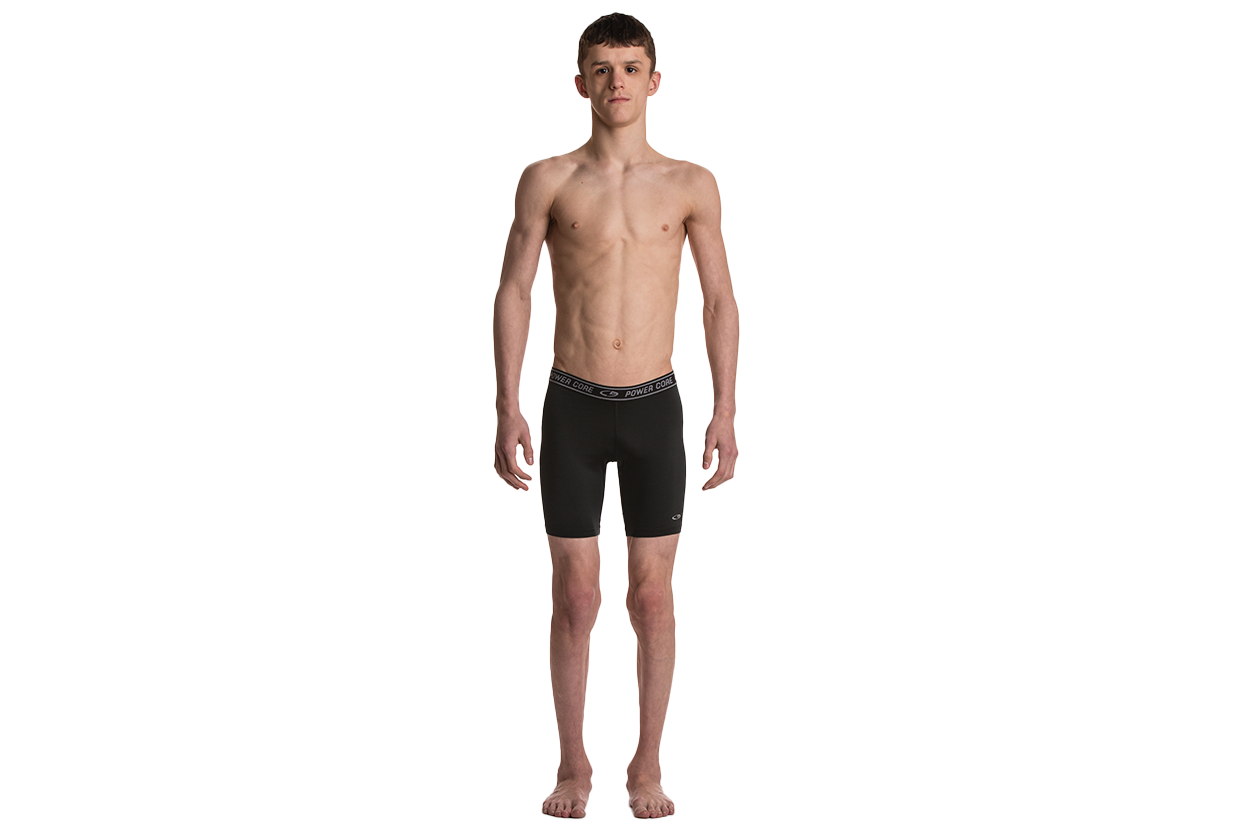
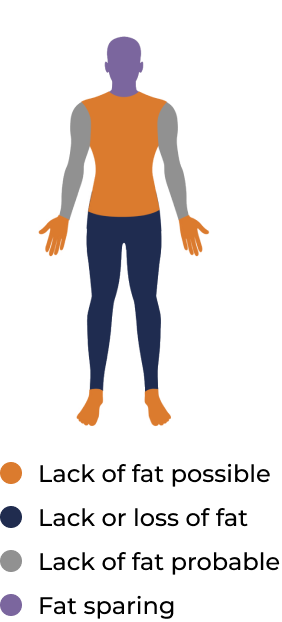
All types of GL (congenital and acquired forms) are characterised by loss of subcutaneous fat over the whole body. Patients with GL usually appear very thin and mostly have a muscular appearance. (hyperlink the generalised and partial lipodystrophy, as we did in the intro section).

Partial lipodystrophy (GL)
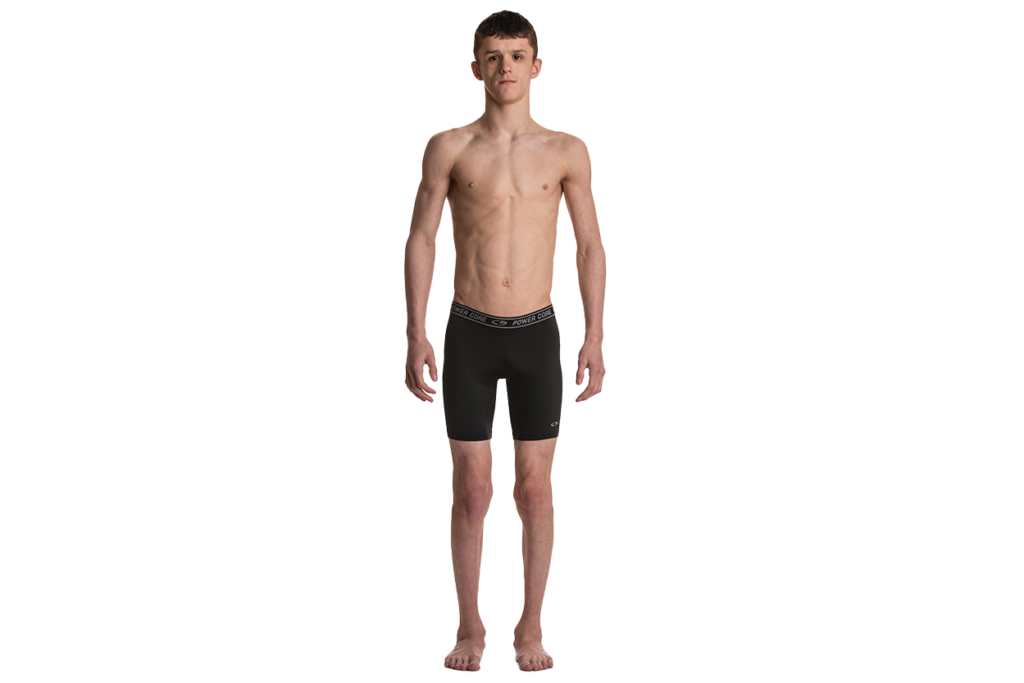
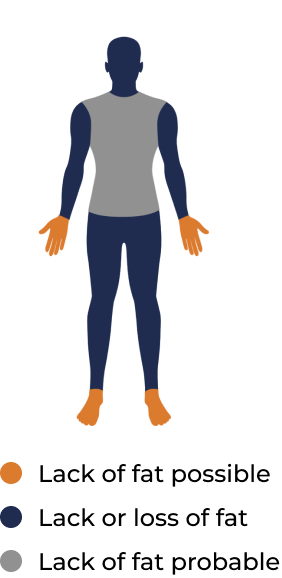
With PL, especially the familial form, the loss of subcutaneous fat may not be obvious. There can be normal amounts of fat or fat accumulation in some parts of the body and loss in others. In most cases with FPLD, fat loss predominantly affects the lower parts of the body. Accumulation of fat can be seen around the face and neck in some patients
GENERALISED LIPODYSTROPHY
- Generalised absence of subcutaneous adipose tissue
- Resulting deficiency in the hormone leptin
- Metabolic abnormalities including
- Insulin resistance
- Diabetes mellitus
- Hypertriglyceridemia
- Ectopic fat deposition in the liver, muscle, and other organs which may cause serious organ damage
- Estimated prevalence 0.23-0.96 in 1,000,000 population
- May be Congenital – from birth or Acquired – usually presenting in childhood or adolescence
Congential
Characteristics of Congenital Generalised Lipodystrophy
Age of onset: Apparent at birth or early childhood
Male : Female ratio: 1 : 1 – 2
Essential characteristics:
- Autosomal recessive (AR) inheritance in vast majority of cases,
- Family history or consanguinity may present
- Near-complete lack of adipose tissue
Possible clinical features of Congenital Generalised Lipodystrophy
Not all of these features may be present in all patients:
- Hyperphagia
- Prominent muscles and veins
- Hepatosplenomegaly
- Hyperlipidemia
- Acanthosis nigricans, signs of insulin resistance, diabetes
- Hyperandrogenism in females
- Acromegaloid features
- Advanced bone age Accelerated growth
Acquired
Characteristics of Acquired Generalised Lipodystrophy
Age of onset: Variable, usually in childhood or adolescence
Male : Female ratio: 1 : 3
Essential characteristics:
- Progressive loss of fat leading to near-complete lack of adipose tissue
- No family history
- Associated with autoimmune illness e.g. juvenile dermatomyositis, autoimmune hepatitis, type 1 diabetes or panniculitis
Possible clinical features of Acquired Generalised Lipodystrophy
Not all of these features may be present in all patients:
- Variable fat loss pattern (e.g. preserved intra-abdominal fat in some cases)
- Hyperphagia
- Prominent muscles and veins
- Hepatosplenomegaly
- Hyperlipidemia
- Acanthosis nigricans, signs of insulin resistance, diabetes
- Hyperandrogenism in females
PARTIAL LIPODYSTROPHY
- Generalised absence of subcutaneous adipose tissue
- Resulting deficiency in the hormone leptin
- Metabolic abnormalities including
- Insulin resistance
- Diabetes mellitus
- Hypertriglyceridemia
- Ectopic fat deposition in the liver, muscle, and other organs which may cause serious organ damage
- Estimated prevalence 0.23-0.96 in 1,000,000 population
- May be Congenital – from birth or Acquired – usually presenting in childhood or adolescence
Congential
Characteristics of Familial Partial Lipodystrophy
Age of onset: Around puberty
Male : Female ratio: 1 : 4 – 5
Essential characteristics:
- Regional loss of adipose tissue.
- Compensatory excess common, may resemble obesity or Cushing’s Syndrome
- May present with hyperphagia
- Variable degree of metabolic abnormalities
Possible clinical features of Familial Partial Lipodystrophy
FPLD more likely to present with:
- Hyperphagia
- Prominent muscles and veins
- Acanthosis nigricans, signs of insulin resistance
- Hyperandrogenism in females
- Pain and mood disorders are frequently reported in PL patients
- Fat loss common in FPLD palms/soles
Acquired
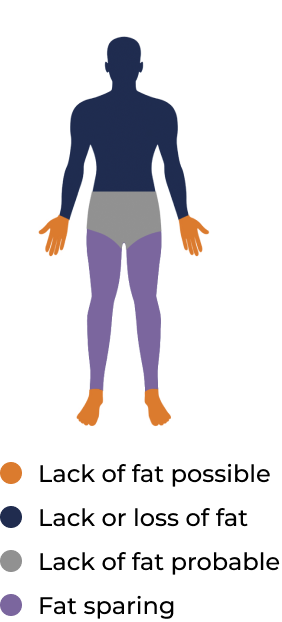
Characteristics of Acquired Partial Lipodystrophy
Age of onset: Child, adolescence or early adulthood
Male : Female ratio: 1 : 4
Essential characteristics:
- Gradual loss of adipose tissue from head downwards
- Fat accumulation around the hips, buttocks, legs.
- Metabolic abnormalities less common, but can vary in severity
Possible clinical features of Acquired Partial Lipodystrophy
APLD more likely to present with:
- No fat loss from lower extremities
- Fat accumulation: hips, buttocks, lower limbs
- Mild or no metabolic complications (but these may still be found)

Due to its complex and often little-known conditions, lipodystrophy can be considered to be a disease with many faces that is often diagnosed very late. Although lipodystrophy cannot be cured there are some treatment possibilities for the complications available.